Pediatric anesthesiology 2016 reviews
Session I: Regional Anesthesia - "Comfortably Numb"
Reviewed by Jorge Gálvez, MD
The Children’s Hospital of Philadelphia
University of Pennsylvania, Perelman School of Medicine
One of the highlights of the meeting was the session on neuraxial adjuvants/ anesthesia and regional anesthesia.
The opening lecture titled “Neuraxial Anesthetic Adjuvants” by Tony Yaksh, Ph.D. (University of California, San Diego) highlighted the importance of research to establish the safety and therapeutic profile of neuraxial medications in pediatric populations. To date, none of the agents in clinical use for neuraxial anesthesia or analgesia (either intrathecal or epidural) have been approved by the FDA for pediatric use in the United States. All commentaries discussed in his lecture reflected off-label use of these medications in children. The dosing regiments used are not clinically validated in safety studies.
He further stressed the importance of this issue by highlighting major journals involved in pain and anesthesia research. Publishing guidelines require that systematic pre-clinical safety should be established or specific FDA approval gained before undertaking trials that apply off-label use of medications, such as neuraxial administration of analgesics or adjuvant analgesics to children(1).
Neonatal and infant populations are inherently undergoing neurodevelopment. There may be vulnerable periods during neurodevelopment that are unique to these populations. Agents that modulate neuronal activity may have effects that are unique to pediatric populations in contrast with adult populations. Without safety and toxicology research, it is not possible to determine the answer to these important questions. Quoting Dr. Yaksh, “Just because it’s safe in adults doesn’t mean it’s safe for children.”
Dr. Yaksh described animal models to simulate neonatal medication administration, some of which were developed in his laboratory. One of the challenges of these animal models is that the biologic effect (analgesia) is difficult to determine (2, 3).
In these cases, we may not be able to identify the extent of analgesia on the therapeutic spectrum. This limits the ability to determine the therapeutic margin for specific medications based on the animal models. Based on his research on neonatal rats, intrathecal ketamine resulted in neurodegeneration and apoptosis based post-mortem evaluation. These findings were in contrast with intrathecal morphine, clonidine, and bupivacaine, neither of which caused detectable apoptosis or neurodegeneration. All three agents were associated with analgesia in the rat model.
In conclusion, Dr. Yaksh stressed the importance of conducting appropriate pre-clinical assessments for pediatric neuraxial medications. His laboratory has validated a rat model for neuraxial medication evaluation based on P3 and P7 neonatal rats. He noted a common saying in pharmacology and toxicology: “there are no safe drugs, only safe doses.” Dr. Yaksh concluded his presentation with a call to action for funding agencies and societies like SPA to support research on safety and efficacy of analgesic and anesthetic agents for children and infants.
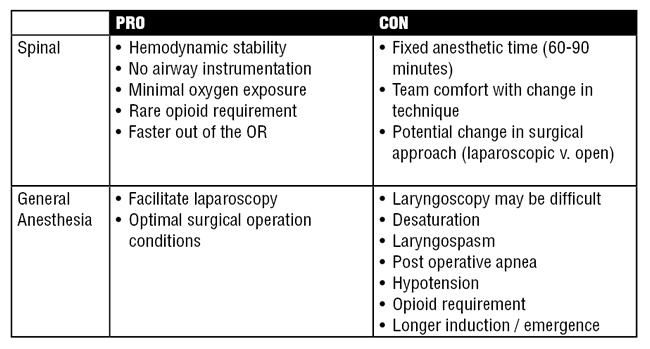
The second presentation, “Neonatal Spinals and Caudals” by Robert Williams, MD (University of Vermont, Burlington), described the clinical considerations for neuraxial anesthesia for infants and children. He focused on describing the potential advantages of infant spinal anesthesia regarding cardiovascular stability, hypoxemia, postoperative apnea and potential risks of anesthetic neurotoxicity. Furthermore, he described the types of surgical procedures amenable to infant spinal anesthesia.
Infant spinal anesthesia is not a new concept. In fact, incorporating infant spinal anesthesia instead of general anesthesia for surgical procedures may require more of a change in the mindset rather than the skillset for all involved. In Burlington, the medical and patient community have embraced the practice of spinal anesthesia on infants as the sole anesthetic for various surgical procedures in the lower abdomen and lower extremities that last less than one hour (4). This practice was recently highlighted by a patient story on the Wall Street Journal. A video interview can be found here.
Regarding the topic of anesthetic neurotoxicity, Dr. Williams quoted the recently published GAS trial. To date the trial has not demonstrated any neurodevelopmental differences between infants that received general anesthesia versus spinal anesthesia at two years of age. However, the trial did report improved hemodynamic stability, respiratory stability (less apnea, hypoxemia)(5).
It has been the only anesthetic technique associated with reduced incidence of postoperative apnea in preterm infants and other at-risk populations.(6) Davidson et al. recently reported on early versus late apnea following surgical hernia repair on premature infants (conceptual age 26 weeks or less). The study found that 2% of infants that received either regional anesthesia or general anesthesia might develop apnea within 12 hours of surgery.
One of the potential risks of spinal anesthesia is that it fails to achieve adequate surgical anesthesia.(7) More importantly, planning for the management of patients with a failed spinal is arguably one of the most important considerations for the pre-operative discussion and intra-operative management. At Vermont, patients are counseled that in the event that the spinal is not successful, the procedure will be canceled and re-scheduled for a later date. This decision has been reached unanimously between surgeons, anesthesiologists, perioperative nurses, pediatricians and neonatologists. Pediatric anesthesiologists must always be prepared to provide respiratory support to infants following spinal anesthesia. Dr. Williams commented that an important finding of the GAS trial is infant spinal anesthesia can be achieved effectively throughout the world.
Regarding the practical aspects, Dr. Williams described experience with tetracaine, ropivacaine, hyperbaric and isobaric bupivacaine. He did not advocate any specific agent, but did quote the published protocol in the GAS trial, which has been successful at various sites around the world. This protocol consists of isobaric bupivacaine 0.5% (0.2mL/kg) with a maximum dose of 4.5 to 5.0mg using either a 22g or 25g spinal needle. This dose may achieve 60 to 90 minutes of surgical anesthesia.
Similar to adult neuraxial anesthesia, good positioning is critical to the success of inserting the spinal. They describe a technique where the infant is sitting facing the assistant. The assistant places both thumbs on the infant’s shoulders and the pinky fingers behind the infant’s knees. The remaining fingers are along the thorax and abdomen and assist to stabilize the infant. The assistant hugs the infant while the back is prepped with betadine. Oral dextrose solution, or “sweeties”, can be used during spinal placement and subsequently during the surgical procedure to keep the baby happy and occupied(8).
Once the spinal is completed, the baby is positioned supine and a lower extremity peripheral intravenous line is inserted. Providers may be able to place an intravenous line before or after the spinal based on individual evaluation of the patient. During surgery, the anesthesiologist continues to interact with the baby by holding hands, or perhaps providing a pacifier with “sweeties”. One of the clear benefits of spinal anesthesia is that there is no time required for emergence, extubation and stabilization of the patient prior to transport from the operating room. This may reflect a lateral trade in terms of time. There will always be times that the spinal will be difficult, just like the airway may be difficult.
The final speaker of the session, Giovanni Cucchiaro, MD (Children's Hospital Los Angeles), reviewed the current evidence supporting the practice of neuraxial and regional approaches for surgical anesthesia and postoperative analgesia for children and adolescents. Before jumping to adopt the newest block, consider the following:
- If you want to change your practice, which practice does it (the new technique) work better on?
- What are you trying to achieve?
- Why are you interested in changing what you have been doing for years?
Dr. Cucchiaro provided a thoughtful and comprehensive overview of neuraxial and peripheral nerve blocks that offer analgesia for overlapping anatomic distribution.
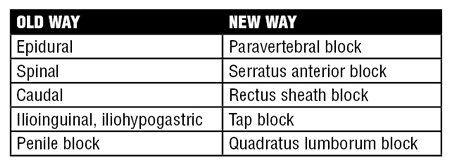
Paravertebral block
The paravertebral block involves infiltration of local anesthetic along the spinal nerve roots. The block provides cutaneous and visceral analgesia. Each paravertebral level targeted may achieve local anesthetic spread of 2-3 levels. Usually, the local anesthetic spread in caudal direction more than the cephalad direction. As a result, the sensory block is wider. However, in almost 30% of patients, the local anesthetic spread may not be sufficient. In contrast with epidural block, paravertebral blocks may not achieve the same range of anesthesia. To date, there is no convincing data supporting single shot paravertebral block over epidural. Continuous infusion may be more effective with an epidural catheter. Paravertebral blocks may be used for abdominal surgery, but must be performed bilaterally to achieve adequate anesthesia. In contrast with epidural analgesia, two paravertebral catheters would be required to achieve comparable analgesia. This may be associated with variable performance of one catheter over the other.
Dr. Cucchiaro also referenced the ongoing work through the Society for Pediatric Anesthesia Improvement Network (SPAIN) on evaluating various analgesic strategies for patients undergoing Nuss bar procedures. Currently, the group is evaluating outcomes for this group of patients receiving epidural, paravertebral, or multi-modal analgesia. For additional information regarding this project, please see the SPAIN website.
Anesthesiologists have several options for truncal or abdominal wall analgesia, including the rectus sheath block, transverse abdominal plane block, or the iliohypogastric block. Additional description of the procedures may be found on the New York School of Regional Anesthesia (NYSORA) site (This site describes the procedure in adults).
The rectus sheath block may be appropriate for surgical procedures near the umbilicus(9). Several studies have compared local anesthesia infiltration (LAI) to the rectus sheath block.
- Dingeman et al (2013) reported 52 patients ages 3-12 years receiving LAI or a rectus sheath block (10). There was no difference in morphine use between the groups, and the rectus sheath block lasted longer than LAI.
- Gurnaney evaluated the analgesic efficacy of the rectus sheath block versus LAI and found that there were no differences in pain scores in the PACU or afterwards between the groups. However, the LAI group received higher doses of morphine in the perioperative period (11).
- Isaac et al. conducted a pilot study of 14 children ages 1 through 8 years and found no difference in pain scores or analgesic medication consumption between LAI and rectus sheath block(12).
Transverse Abdominal Plane Block (TAP)
The purpose of the TAP block is to achieve analgesia over the abdominal wall. The block offers flexibility, as a subcostal injection may achieve nice spread from lateral side of body towards midline, thus covering an incision in the upper abdomen. Conversely, injection along the mid-axillary line results in analgesia along the lateral aspect of the abdomen and may be more appropriate for a lower abdominal incision.
A Cochrane review by Charlton et al. found various studies comparing TAP and epidural blocks with variable patient enrollment, methodological differences and other methodological inconsistencies(13). In general, TAP block compared to placebo or conventional therapy demonstrated similar morphine requirements at 2 hours, but reduced morphine consumption over the first 24 hours. Furthermore, the TAP block is generally associated with prolonged time to first request of analgesia. There were no differences in postoperative nausea or vomiting. The practice in children may be different, and TAP performance may be better for certain urologic procedures. There is ongoing work in this area to define the optimal application of the TAP block in a pediatric surgical practice.
The serratus block can be used to provide paresthesia to the hemithorax. The technique targets the thoracic intercostal nerves along T2 and T12 as well as the lateral cutaneous branches over the antero-lateral chest wall. The block can be performed along the superficial serratus plane, located between the pectoralis major and minor. Alternatively, the deep serratus plane is located underneath the serratus muscle, but above the ribs, typically at the level of the 4th and 5th ribs(14).
Quadratus Lumborum Block
The quadratus lumborum block is suitable for analgesia of the intra-abdominal viscera(14). Local anesthetic spread varies depending on whether the needle is positioned in anterior or posterior to the quadratus lumborum. Carney et al. demonstrated local anesthetic spread concentrates near the vertebral body, but did not find any spread toward the paravertebral space(15).
Dr. Cucchiaro concluded his presentation with more questions than answers. He quoted Leonardo Da Vinci: “Life is pretty simple. You do some stuff. Most fails. Some works. You do more of what works. If it works big, others quickly copy. Then you do something else. The trick is the doing something else.” There are many variations to regional anesthesia practice, which should be taken into consideration when evaluating a new technique at any institution. This may be especially true for some of the abdominal and truncal regional blocks, since there may be important variations in local anesthetic spread depending on the technique employed. Last, Dr. Cucchiaro highlighted the importance of ongoing research to evaluate optimal techniques. In Da Vinci’s words, “The greatest deception men suffer is from their own opinions."
References
- Tobin JR, Shafer SL, Davis PJ. Pediatric research and scholarship: another Gordian knot? Anesth Analg. 2006;103(1):43-8.
- Walker SM, Westin BD, Deumens R, Grafe M, Yaksh TL. Effects of intrathecal ketamine in the neonatal rat: evaluation of apoptosis and long-term functional outcome. Anesthesiology. 2010;113(1):147-59.
- Westin BD, Walker SM, Deumens R, Grafe M, Yaksh TL. Validation of a preclinical spinal safety model: effects of intrathecal morphine in the neonatal rat. Anesthesiology. 2010;113(1):183-99.
- Williams RK, Adams DC, Aladjem EV, Kreutz JM, Sartorelli KH, Vane DW, et al. The safety and efficacy of spinal anesthesia for surgery in infants: the Vermont Infant Spinal Registry. Anesth Analg. 2006;102(1):67-71.
- Davidson AJ, Disma N, de Graaff JC, Withington DE, Dorris L, Bell G, et al. Neurodevelopmental outcome at 2 years of age after general anaesthesia and awake-regional anaesthesia in infancy (GAS): an international multicentre, randomised controlled trial. Lancet. 2016;387(10015):239-50.
- Davidson AJ, Morton NS, Arnup SJ, de Graaff JC, Disma N, Withington DE, et al. Apnea after Awake Regional and General Anesthesia in Infants: The General Anesthesia Compared to Spinal Anesthesia Study--Comparing Apnea and Neurodevelopmental Outcomes, a Randomized Controlled Trial. Anesthesiology. 2015;123(1):38-54.
- Frawley G, Bell G, Disma N, Withington DE, de Graaff JC, Morton NS, et al. Predictors of Failure of Awake Regional Anesthesia for Neonatal Hernia Repair: Data from the General Anesthesia Compared to Spinal Anesthesia Study--Comparing Apnea and Neurodevelopmental Outcomes. Anesthesiology. 2015;123(1):55-65.
- Marcatto Jde O, Tavares EC, Silva YP. Benefits and limitations of the use of glucose for the treatment of pain in neonates: a literature review. Rev Bras Ter Intensiva. 2011;23(2):228-37.
- Mori H, Akita K, Hata Y. Anatomical study of innervated transverse rectus abdominis musculocutaneous and deep inferior epigastric perforator flaps. Surg Radiol Anat. 2007;29(2):149-54.
- Dingeman RS, Barus LM, Chung HK, Clendenin DJ, Lee CS, Tracy S, et al. Ultrasonography-guided bilateral rectus sheath block vs local anesthetic infiltration after pediatric umbilical hernia repair: a prospective randomized clinical trial. JAMA Surg. 2013;148(8):707-13.
- Gurnaney HG, Maxwell LG, Kraemer FW, Goebel T, Nance ML, Ganesh A. Prospective randomized observer-blinded study comparing the analgesic efficacy of ultrasound-guided rectus sheath block and local anaesthetic infiltration for umbilical hernia repair. Br J Anaesth. 2011;107(5):790-5.
- Isaac LA, McEwen J, Hayes JA, Crawford MW. A pilot study of the rectus sheath block for pain control after umbilical hernia repair. Paediatr Anaesth. 2006;16(4):406-9.
- Charlton S, Cyna AM, Middleton P, Griffiths JD. Perioperative transversus abdominis plane (TAP) blocks for analgesia after abdominal surgery. Cochrane Database Syst Rev. 2010(12):CD007705.
- Blanco R, Parras T, McDonnell JG, Prats-Galino A. Serratus plane block: a novel ultrasound-guided thoracic wall nerve block. Anaesthesia. 2013;68(11):1107-13.
- Carney J, Finnerty O, Rauf J, Bergin D, Laffey JG, Mc Donnell JG. Studies on the spread of local anaesthetic solution in transversus abdominis plane blocks. Anaesthesia. 2011;66(11):1023-30.